According to findings presented at the 2021 ASH Annual Meeting, the combination of daratumumab, carfilzomib, lenalidomide, and dexamethasone (Dara-KRd), autologous hematopoietic cell transplantation (AHCT), and response-adapted consolidation led to high rates of measurable residual disease (MRD) negativity in newly diagnosed multiple myeloma. The researchers noted that the high rate of patients who remained MRD-negative despite cessation of treatment suggests MRD surveillance could be an alternative to indefinite maintenance treatment.
In their study, researchers evaluated the safety and clinical activity of Dara-KRd and assessed MRD’s utility to inform the use and duration of the combination regimen following AHCT and to guide treatment cessation in patients with MRD negativity.
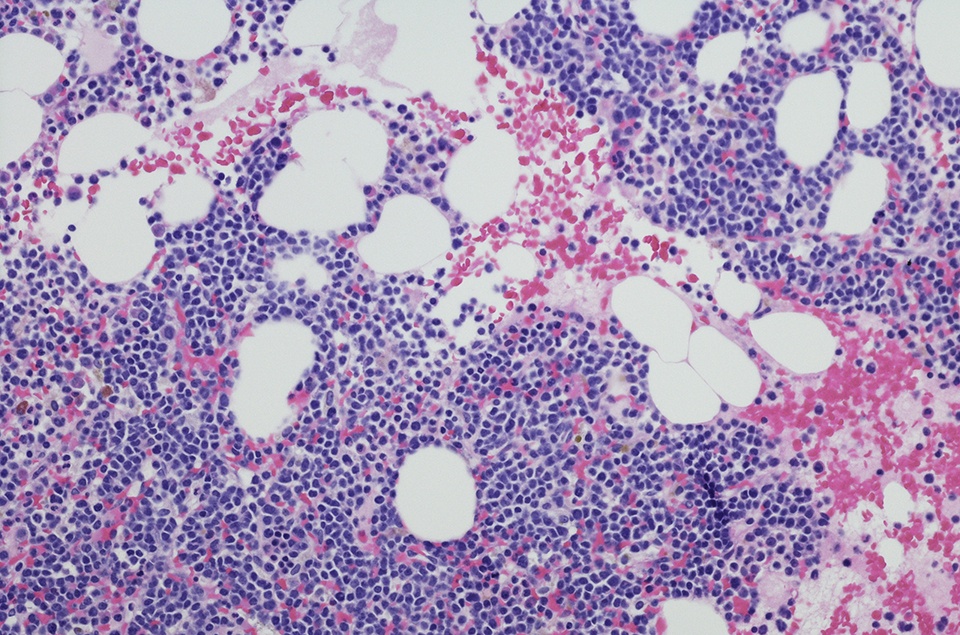
The study included 123 patients with newly diagnosed myeloma who required treatment. Patients had a CrCl ≥40 ml/min, adequate liver and heart function, and an Eastern Cooperative Oncology Group performance status of 0 to 2.
Dara-KRd treatment included:
- intravenous daratumumab 16 mg/kg on days 1, 8, 15, and 22
- intravenous carfilzomib 56 mg/m2 on days 1, 8, and 15
- oral lenalidomide 25 mg on days 1-21
- oral/intravenous dexamethasone 40 mg on days 1, 8, 15, and 22
Treatment was repeated every 28 days. Patients received four cycles of Dara-KRd as induction, AHCT, and 0, four, or eight cycles of Dara-KRd consolidation, according to MRD status.
The investigators assessed MRD by next-generation sequencing in patients at the end of induction, following AHCT, and during each four-cycle block of Dara-KRd consolidation. The primary endpoint in the intent-to-treat study population was achievement of MRD negativity (<10-5). Additionally, the investigators also assessed MRD <10-6, as well as complete response.
Treatment was administered until patients showed two consecutive MRD measurements of <10-5. Patients with confirmed MRD negativity entered a treatment-free observation and MRD surveillance phase. Surveillance was performed for MRD resurgence at six months following treatment cessation and annually thereafter. Lenalidomide was administered as maintenance therapy in patients who completed consolidation without confirmed MRD negativity.
Approximately 43% of patients (n=53) had no high-risk cytogenetic abnormalities, while 37% (n = 46) had one and 20% (n=24) had two or more high-risk cytogenetic abnormalities. Cytogenetic abnormalities reported in the study population included gain 1q, t(4;14), t(14;16), t(14;20), or del17p. Patients’ median age was 60 years (range = 36-79), and around 20% were 70 years of age or older.
The median follow-up was 25.1 months. At time of data reporting, four patients were still on the protocol treatment, while 20 patients transitioned to lenalidomide maintenance and 84 have experienced MRD negativity and entered the treatment-free observation and MRD surveillance phase. For the latter group of patients, the median follow-up after treatment cessation was 14.2 months. The most frequently reported severe adverse events in these patients included pneumonia (n = 8) and venous thromboembolism (n = 3). A total of three patients died during therapy.
Most patients (80%) had achieved MRD negativity, and 66% had achieved MRD <10-6. According to the researchers, the depth of response improved at each therapy phase and became comparable among groups with no, one, or two or more high-risk abnormalities.
The two-year progression-free survival (PFS) rate was 87%, which included rates of 91% in patients with no high-risk cytogenetic abnormalities, 97% in those with one, and 58% in patients with two or more high-risk cytogenetic abnormalities. Additionally, the two-year overall survival (OS) rate was 94%, which included 96%, 100%, and 75% in patients with no, one and two or more high-risk cytogenetic abnormalities, respectively.
“While most patients with ultra-high risk myeloma reach deep responses with this approach, novel consolidative strategies are needed,” the authors concluded. “For most patients with newly diagnosed myeloma, this strategy creates the opportunity of MRD surveillance as an experimental alternative to the burden of indefinite maintenance.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.