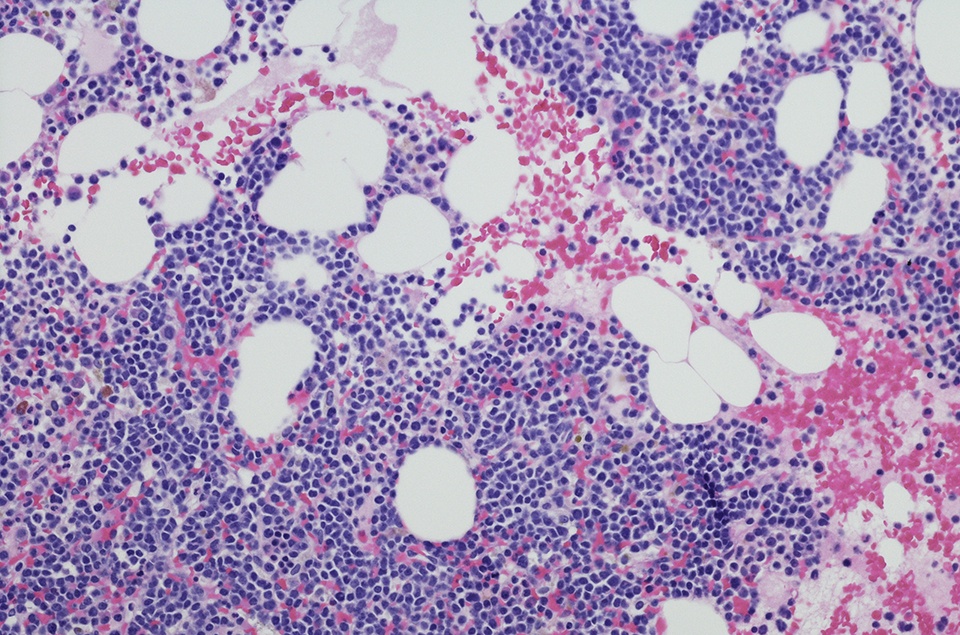
According to results from the phase III BELINDA trial, patients with relapsed/refractory aggressive B-cell non-Hodgkin lymphoma (NHL) who received the autologous CD19-targeting chimeric antigen receptor (CAR) T-cell therapy tisagenlecleucel (tisa-cel) as second-line treatment experienced event-free survival (EFS) that was noninferior to standard platinum-based chemotherapy (PCT). Lead author Michael R. Bishop, MD, shared these findings at the 2021 ASH Annual Meeting.
The BELINDA trial randomized 322 adults with relapsed/refractory aggressive B-cell NHL to receive either tisa-cel (arm A; n = 162) or standard of care (arm B; n = 160).
Patients in arm A received investigator’s choice of protocol-defined PCT regimens as optional bridging therapy, followed by lymphodepletion and a single infusion of tisa-cel (0.6-6×108 CAR T cells/kg). In arm B, patients received investigator’s choice of PCT regimen followed by either autologous hematopoietic cell transplantation (autoHCT) for those whose disease responded to the treatment or second PCT for those whose disease did not respond. Disease assessments were performed at six and 12 weeks. Week six assessments evaluated disease burden prior to tisa-cel infusion (and after bridging, if applicable) in arm A, and determined whether responses were sufficient for autoHCT or if a second PCT regimen was required in arm B.
Two-thirds of patients in each arm had primary refractory disease, and more patients in arm A had high-grade B-cell lymphomas (24% vs. 17%) and International Prognostic Index score ≥2 (65% vs. 58%). The primary endpoint of the study was EFS, defined as the time from randomization to stable disease (SD) or progressive disease (PD) at or after the 12-week assessment, or death at any time.
At a median follow-up of 10 months (range = 2.9-23.2), the median EFS in both treatment arms was three months (hazard ratio [HR] = 1.07; p = 0.69). In arm A, patients who presented with PD at week six had shorter EFS. While certain patients responded to tisa-cel after SD or PD without additional treatment at the week 12 assessment, the EFS analysis considered this an event.
Eighty-four percent of patients in arm A experienced a grade ≥3 adverse event (AE), (compared with 90% in arm B. AEs included grade ≥3 cytokine release syndrome (CRS) in 5% and grade ≥3 neurologic events in 3% of tisa-cel recipients. During the study period, 52 (32%) and 45 (28%) deaths occurred in arms A and B, respectively. The most common cause of death in each group was PD, followed by AEs.
The authors noted several limitations with this analysis, including “design elements, such as optional PCT bridging therapy in arm A with potential delay of tisa-cel infusion until after week six assessment, allowance of a different PCT regimen to reach autoHCT in arm B after inadequate response to first PCT, and imbalances in relevant patient characteristics.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.