For years, the standard prophylaxis for graft-versus-host disease (GVHD) after allogeneic hematopoietic cell transplantation (HCT) has been a calcineurin inhibitor, such as tacrolimus, and methotrexate. However, according to Shernan Holtan, MD, efforts to intensify immunosuppressive regimens often lead to higher risk of serious infection and relapse, and though they may improve acute GVHD, they typically do not improve rates of chronic GVHD.
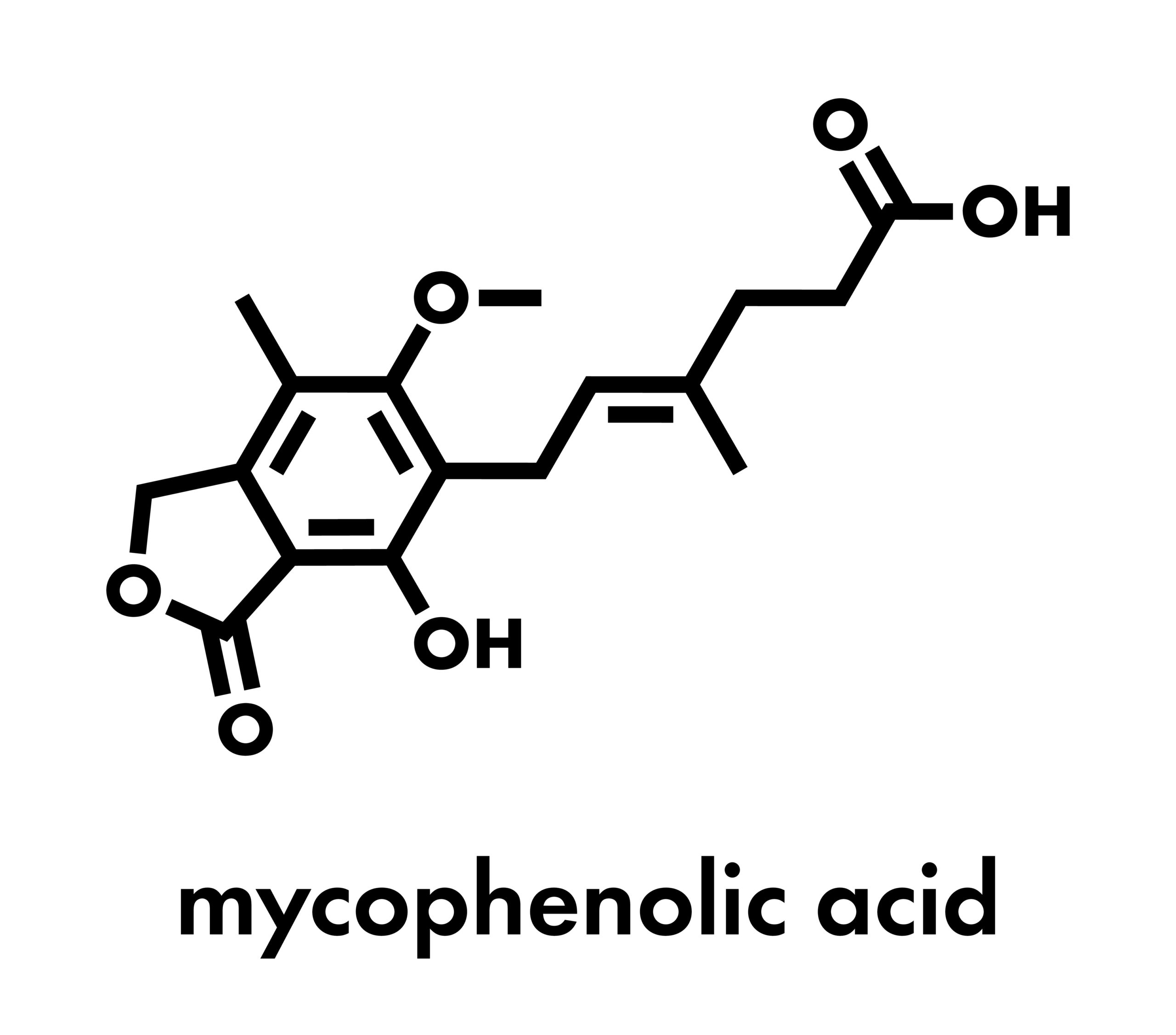
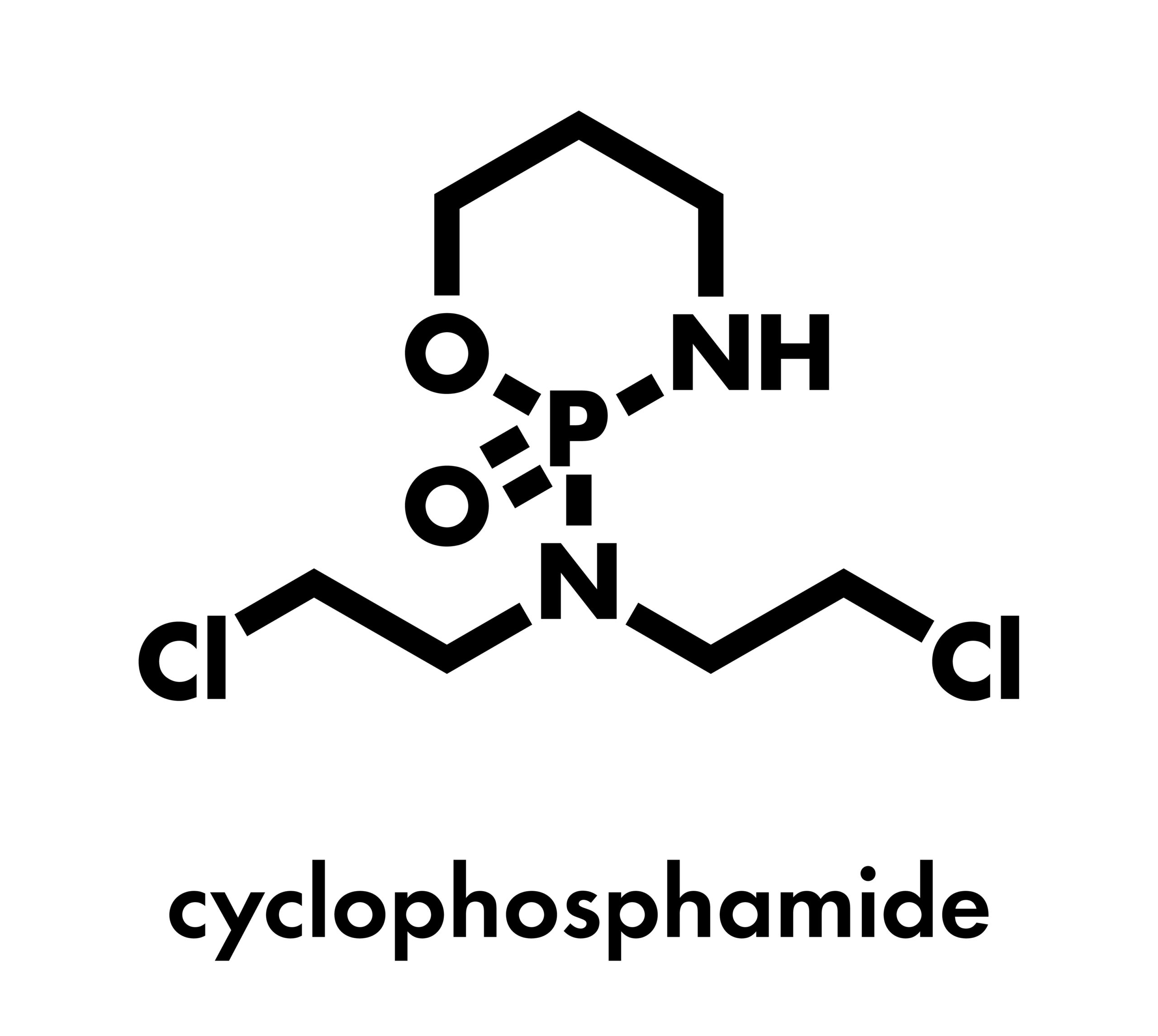
Dr. Holtan and colleagues evaluated a new GVHD prophylaxis regimen consisting of posttransplant cyclophosphamide (PTCy), tacrolimus, and mycophenolate mofetil (MMF). They concluded that PTCy, tacrolimus, and MMF improved GVHD-free, relapse-free survival (GRFS) at 1 year compared with standard tacrolimus and methotrexate. Their findings were presented as a late-breaking abstract at the 64th ASH Annual Meeting and Exposition.
PTCy, Tacrolimus, and MMF for GVHD Prophylaxis
The phase 3 trial included 431 patients undergoing reduced-intensity conditioning allogeneic HCT. Peripheral blood stem cell graft donors were 6 of 6 human leukocyte antigen (HLA) matched related for 128 patients, 8 of 8 matched unrelated for 288 patients, and 7 of 8 single mismatched for 15 patients. A total of 214 patients received PTCy, tacrolimus, and MMF, while 217 received tacrolimus and methotrexate. The study’s primary end point was GRFS, and secondary end points included incidence of acute and chronic GVHD, engraftment, relapse or progression, infection, and survival.
Reportedly, the PTCy arm had a significantly lower risk for GRFS events compared with the standard regimen arm (hazard ratio [HR], 0.641; 95% CI, 0.492-0.835; P=.001). Specifically, the PTCy group had an adjusted 1-year GRFS rate of 52.7% (95% CI, 45.8-59.2) compared with 34.9% in the standard arm (95% CI, 28.6-41.3). Dr. Holtan explained that the reduced GRFS in the PTCy arm was due to a reduction in both acute and chronic GVHD compared with the control arm.
The authors did note that there was no significant difference in rates of relapse or progression and overall survival at 1 year. In addition, rates of grade 3 infections were similar between the groups (12.2% vs 13.3%; P=.8), though rates of grade 2 infections were higher with the PTCy regimen (33.7% vs 23.5%; P=.002), and there was no difference in cytomegalovirus reactivation (7.3% vs 7.1%; P=.8).
The researchers suggested that PTCy, tacrolimus, and MMF, “which has become standard of care for mismatched transplants, should also become the standard of care for GVHD prophylaxis from closely matched donors receiving reduced-intensity conditioning.”
More From SUO: Adding Itacitinib to Conventional GVHD Prophylaxis




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.