Percutaneous coronary intervention (PCI) with a bioresorbable vascular scaffold (BVS) in mild non-flow-limiting lesions with large plaque burden was found to be safe and substantially enlarged luminal area, according to research presented at Transcatheter Cardiovascular Therapeutics (TCT) 2020.
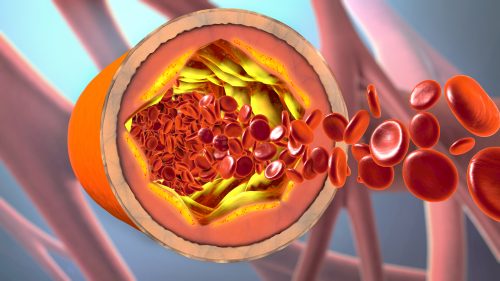
Acute coronary syndromes (ACS) commonly arise from rupture and thrombosis of thincap lipid-rich coronary atheromas with large plaque burden. Thickening the fibrous cap on these lesions with a scaffold or stent treatment may help to normalize wall stress and stabilize high-risk plaque.
PROSPECT ABSORB, a pilot randomized trial part of the PROSPECT II natural history study, examined the outcomes of PCI on non-flow-limiting vulnerable plaques. The trial enrolled 182 patients from PROSPECT II who were screened for at least one non-flow-limiting nonculprit coronary lesion (NCL) with ≥65% plaque burden. Qualifying lesions (1 per patient) were randomized (1:1) to treatment with an Absorb bioresorbable vascular scaffold (BVS) plus Guideline Directed Medical Therapy (GDMT) or GDMT alone. All patients underwent 3-vessel angiography and NIRS-IVUS imaging at 25 months. At baseline, there were no significant differences between groups in regard to overall plaque burden or high-risk plaque characteristics. The primary endpoint was minimum luminal area (MLA) at the lesion site at follow-up.
At the time of analysis, lesions at the original site that were treated with Absorb BVS plus GDMT achieved an average MLA of 6.9 mm2 compared with 3.2 mm2 at baseline. The MLA for lesions treated with GDMT alone remained stable, from 3.1 mm2 at baseline to 3.0 mm2 at 25 months (P<0.0001). The overall rate of Major Adverse Cardiovascular Events (MACE) for the BVS cohort was 4.3% at 24 months, compared with 10.7% for those who received GDMT alone (P=0.12).
“The favorable randomized lesion-related MACE rates observed after BVS treatment compared with GDMT alone warrants the performance of an adequately powered randomized trial to determine whether PCI treatment of focal vulnerable plaques improves patient outcomes,” the researchers said in their presentation.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.