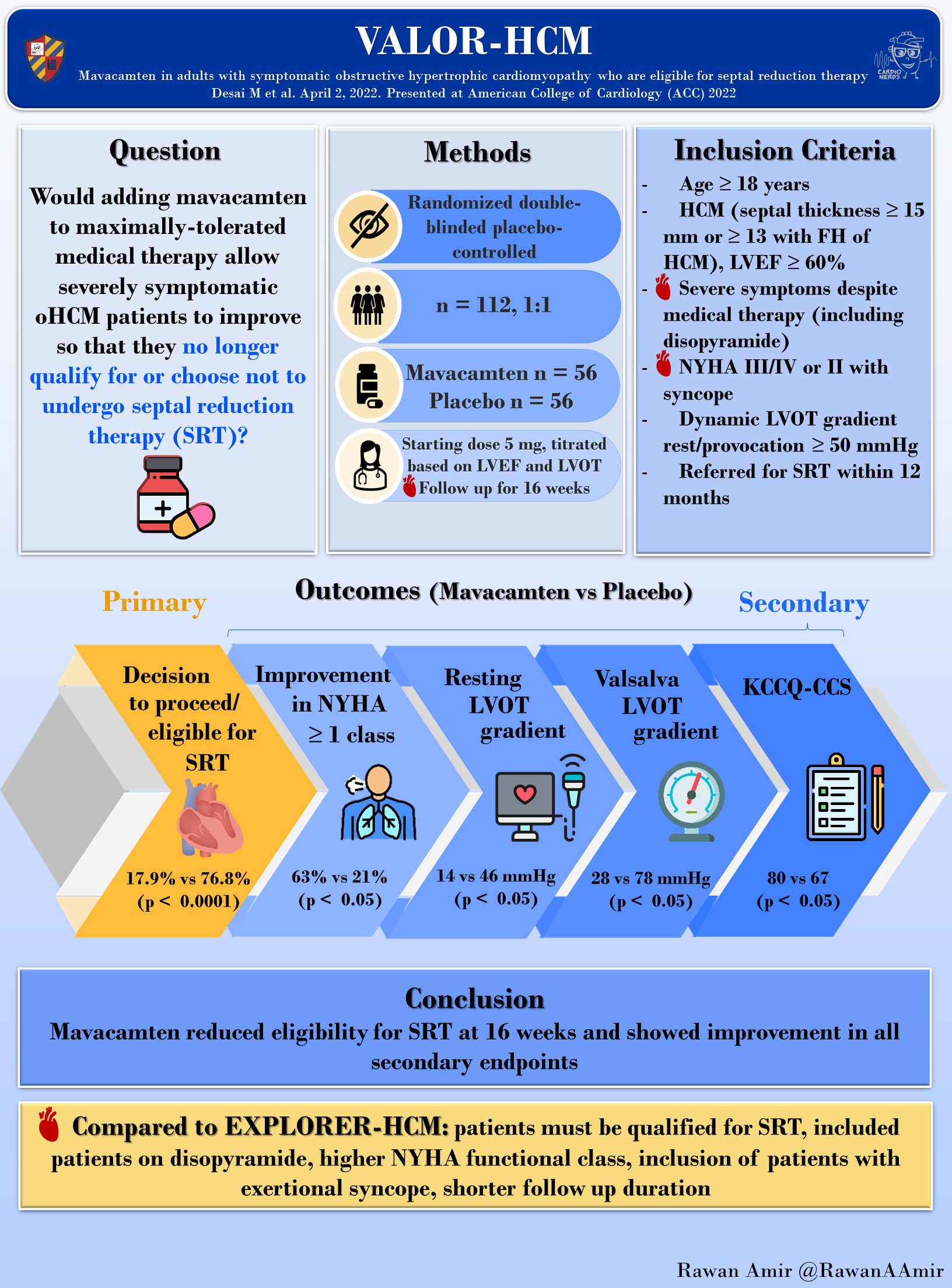
Mavacamten in adults with symptomatic obstructive HCM who are eligible for septal reduction therapy (VALOR-HCM)
Milind Y. Desai, Kathy Wolski, Anjali Owens, Srihari S. Naidu, Jeffrey B. Geske, Nicholas G. Smedira, Hartzell Schaff, Kathy Lampl, Ellen McErlean, Christina Sewell, David Zhang, Jay M. Edelberg, Amy J. Sehnert, Steven E. Nissen, on behalf of VALOR-HCM study investigators*
STUDY RATIONALE: VALOR-HCM
Currently, there are no approved medical therapy alternatives to septal reduction therapy (SRT) for patients with symptomatic drug-resistant obstructive hypertrophic cardiomyopathy. Existing therapies do not address the underlying mechanism of HCM (reduced myocardial compliance and hypercontractility). Mavacamten, a reversible cardiac myosin inhibitor, has shown promise in reducing hypercontractility and improving myocardial compliance. Despite its promise, it has not yet been elucidated if Mavacamten reduces the need for SRT in patients with advanced symptoms.
OBJECTIVE: VALOR-HCM
To assess if Mavacamten is safe and efficacious in reducing the need for SRT when added to maximally tolerated medical therapy among patients with obstructive hypertrophic cardiomyopathy (oHCM).
TRIAL: VALOR-HCM
A randomized, double-blind, placebo-controlled, multicenter (approx. 20 centers in the U.S.), n = 112 participants. Patients were randomized in a 1:1 fashion (n = 56 in Mavacamten group, vs n = 56 in control group. Follow up was 16 weeks.
INTERVENTION: VALOR-HCM
Patients were randomized to either receive placebo or Mavacamten with a starting dose of 5mg, which was titrated using core laboratory measured left ventricular ejection fraction (LVEF) and left ventricular outflow tract (LVOT) gradient at rest and with Valsalva provocation.
OUTCOMES: VALOR-HCM
- Primary Outcome: Composite – decision to proceed with SRT or considered guideline eligible for SRT.
- Secondary Outcomes: Change in postexercise LVOT gradient, NYHA Class, KCCQ-23 CSS, NT-proBNP, and cardiac troponin.
STATISTICAL ANALYSIS: VALOR-HCM
A total sample size of at least 100 patients was needed to provide 95% power to detect a 50% relative difference between groups at a 2-sided αlevel of 0.05. A formal interim analysis was conducted by the iDMC after half of the patients completed the week 16 study visit. Efficacy analyses were performed on the intention to treat population. The comparison of the proportions of patients who met the primary efficacy endpoint between the mavacamten and placebo treatment groups were performed using the Cochran–Mantel–Haenszel test for stratified categorical data. Treatment success was summarized for each treatment group and estimates of group differences with the 95% confidence interval based on normal approximation. A sensitivity analysis was performed to evaluate the number of patients with both improvement of NYHA Class and reduction of all resting and provokable LVOT gradients <50 mmHg. A sequential testing procedure was used for multiplicity control of the secondary endpoints.
RESULTS: VALOR-HCM
- Mean age was 60 years, 49% women, 89% were white, and 92.9% were NYHA class III or higher.
- 46% were on beta blockers, 15% were taking calcium channel blockers, and 32% were on combination therapy. 20% of patients were taking disopyramide.
- Baseline mean LV ejection fraction (LVEF) was 76%. Peak resting LVOT gradient was 49 mmHg and mean post-exercise LVOT gradient was 84 mmHg.
ADVERSE EVENTS: VALOR-HCM
- There were no severe adverse events noted with Mavacamten (no patients experienced chronic heart failure, syncope, or sudden cardiac death)
- 2 patients needing to temporarily stop the drug due to EF falling below 50%.
- There were no permanent discontinuations needed due to EF falling below 30%.
- Non-sustained ventricular tachycardia: 0% vs. 9.1% (Mavacamten vs placebo)
- Nausea: 7.1% vs. 1.8% (Mavacamten vs placebo)
TRIAL CONCLUSIONS: VALOR-HCM
Mavacamten significantly improved symptoms and reduced the need for septal reduction therapy among symptomatic patients with obstructive HCM who were considering SRT and on maximally tolerated medical therapy.
LIMITATIONS & CONSIDERATIONS: VALOR-HCM
- An overwhelming majority of the study participants were white, making the generalizability of the study findings difficult when considering patients of underrepresented backgrounds. A follow-up study assessing the efficacy of Mavacamten in African Americans, Hispanics, and other minority racial groups are necessary.
- The short follow up period of 16 weeks may underestimate the benefits and/or safety of Mavacamten. A longer follow up period is necessary to more accurately determine the efficacy and safety of this novel therapy.
- Trials studying other cardiac myosin inhibitors like Avicamten (REDWOOD-HCM trial NCT04219826) in patients with HCM are underway. Mavacamten has and will create opportunities for other drugs of the similar or same class to be studied in HCM patients.
For background, guidelines, enrollment criteria, outcomes, and references, please visit: #CardsJC: Hypertrophic Cardiomyopathy Trials – EXPLORER-HCM & VALOR-HCM – Cardionerds Twitter Journal Club
Via CardioNerds Academy House Taussig:

CardioNerds Journal Club: a forum for CardioNerds to discuss and breakdown recent publications on twitter, produced with a corresponding infographic and detailed blog post. For more information, check out the CardioNerds Journal Club Page. This Journal Club focuses on the VALOR-HCM Trial.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.