Nonobstructive coronary artery disease, diagnosed by coronary angiography as < 50% epicardial coronary artery stenosis, is a lesser studied form of ischemic heart disease. Stable ischemic heart disease in the absence of obstructive coronary arteries is known as ischemia and nonobstructive coronary artery disease (INOCA). Conversely, acute myocardial infarction (AMI) in the presence of angina or angina equivalent with evidence of ischemia (including troponin elevation) in the absence of obstructive coronary arteries is known as myocardial infarction with nonobstructive coronary arteries (MINOCA). The incidence of MINOCA in patients with AMI ranges from 1-15% (1-3).
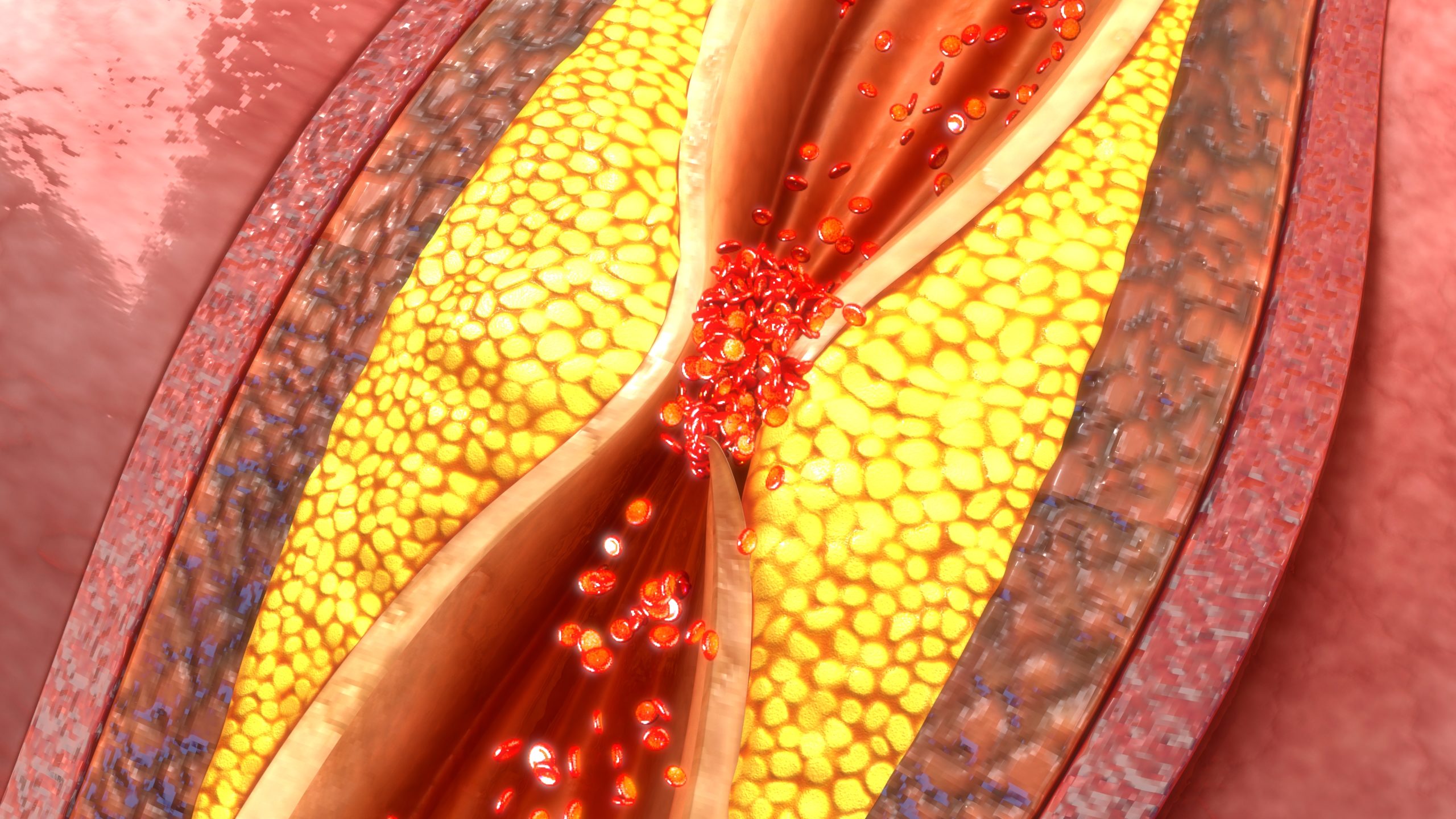
Dr. Martha Gulati, an expert in MINOCA/INOCA, refers to these two entities as syndromes rather than diagnoses at the American Society of Preventive Cardiology (ASPC) 2021 Virtual Summit. She stresses these working diagnoses should not limit further work up as these are not benign diagnoses and portend a higher risk of cardiovascular events independent of other cardiometabolic risk factors per the Women’s Ischemia Syndrome Evaluation (WISE) studies. Proposed underlying mechanisms of INOCA include diffuse atherosclerosis, microvascular dysfunction, and vasospasm. For MINOCA, it is important to rule out not only obstructive coronary artery disease but also nonischemic causes, such as nonischemic cardiomyopathies and myocarditis, and noncardiac causes, such as coagulopathies, systemic inflammation, and metabolic derangements.
Both the European Society of Cardiology (ESC) and the American Heart Association (AHA) recognize the utility of advanced diagnostic imaging to determine the underlying mechanism of MINOCA including plaque erosion/rupture, in-situ thrombosis, spontaneous coronary artery dissection, vasospasm, and endothelial dysfunction. Advanced imaging techniques include invasive coronary reactivity testing, optical coherence tomography (OCT), and cardiac magnetic resonance imaging (CMR). Dr. Gulati emphasizes that by determining the underlying etiology of INOCA/MINOCA with functional and structural imaging studies, better patient risk assessment and outcomes can be obtained.
Treatment of INOCA/MINOCA continues to be an ongoing area of research. While risk factor modification and addressing underlying causes for ischemia remain the cornerstone of treatment, there are select studies which suggest ACEI/ARBs (angiotensin converting enzyme inhibitors and angiotensin receptor blocker) and beta-blockers improve disease management while DAPT (dual antiplatelet therapy) may not be as beneficial. Further investigation remains critical so that targeted therapies can be applied to the different etiologies of this form of ischemic heart disease.
References
- Knuuti J , Wijns W , Saraste A , et al. (ESC Scientific Document Group). 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: the Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J. 2020;41:407–477.
- Reeh J, Therming CB, Heitmann M, et al. Prediction of obstructive coronary artery disease and prognosis in patients with suspected stable angina. Eur Heart J. 2019;40(18):1426-1435.
- Abdu FA, Mohammed AQ, Liu L, Xu Y, Che W. Myocardial Infarction with Nonobstructive Coronary Arteries (MINOCA): A Review of the Current Position. Cardiology. 2020;145(9):543-552. doi: 10.1159/000509100. Epub 2020 Aug 4. PMID: 32750696.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.