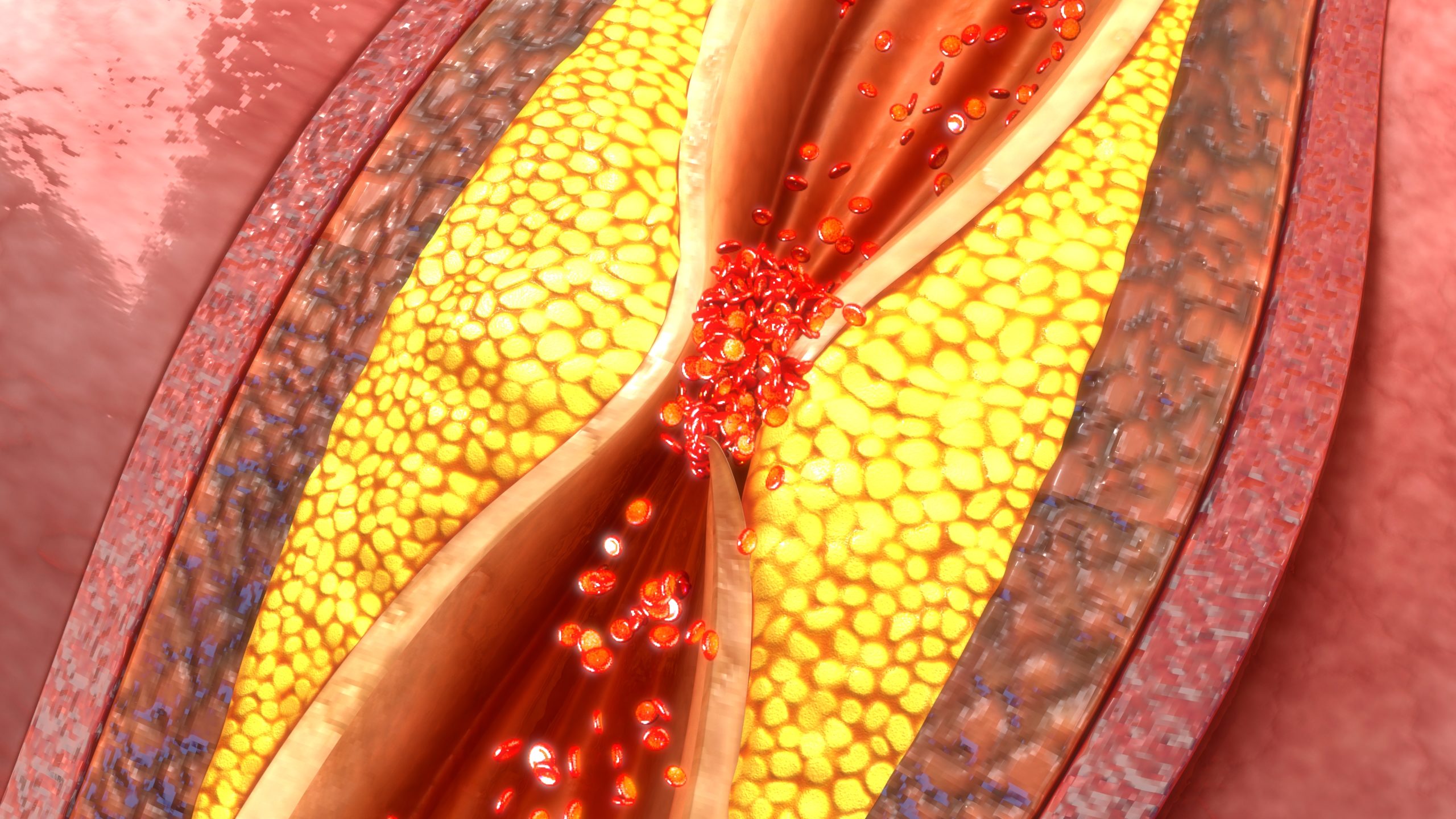
In a recent systematic review and meta-analysis, investigators examined the impact of pre-existing diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), or hypertension (HTN) on the rate of 30-day unplanned readmissions in patients with severe peripheral arterial disease (PAD) who underwent lower extremity bypass (LEB) procedures.
Based on their analyses, the authors found pre-existing DM, CHF, and HTN were associated with increased risk for unplanned hospital readmission within 30 days of LEB. The study was presented in Annals of Vascular Surgery.
Diabetes, Heart Failure, and Hypertension Increase Readmissions
The meta-analysis enrolled 19,739 patients from 5 studies, of which 3559 (18%) were readmitted within 30 days of undergoing LEB for occlusive PAD. The studies were published to the PubMed, Scopus, and Cochrane Library databases by April 2022.
Researchers assessed study quality with GRADE, PRISMA, and ROBINS-I guidelines as well as pooled odds ratios (OR), Q-metric, and Higgins I2 statistics. A total of 4 studies reported on CHF and HTN, 2 studies reported on CAD, and all 5 reported on DM and COPD.
Researchers calculated the following ORs per preexisting comorbidity:
- HTN, 1.35 (95% CI, 1.10-1.64; P<.001; I2=52.20%)
- DM, 1.52 (95% CI, 1.30-1.79; P<.001; I2=74.51%)
- CHF, 1.85 (95% CI, 1.51-2.25; P<.001; I2=50.48%)
- COPD, 1.16 (95% CI, 0.98-1.36; P=.09; I2=61.93%)
- CAD, 1.30 (95% CI, 0.94-1.78; P=.11; I2=51.01%)
Their estimates indicated that DM, HTN, and CHF were statistically significantly associated with an increased risk of 30-day readmission while COPD and CAD were not significantly associated.
Overall, the study’s authors suggested these risk factors could improve patient classification and help elucidate factors that drive hospital readmissions.
Find Related Research on the Peripheral Artery Disease Resource Center






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.