
The T-PASS trial showed that ticagrelor monotherapy after less than 1 month of dual-antiplatelet therapy (DAPT) following percutaneous coronary intervention (PCI) with bioresorbable polymer sirolimus-eluting stents (eg, the Orsiro stent by Biotronik) for acute coronary syndrome (ACS) was both noninferior and superior for a combined ischemic and bleeding outcome when compared with 12 months of DAPT. These provocative results were presented at the 2023 Transcatheter Cardiovascular Therapeutics conference and simultaneously published in Circulation.
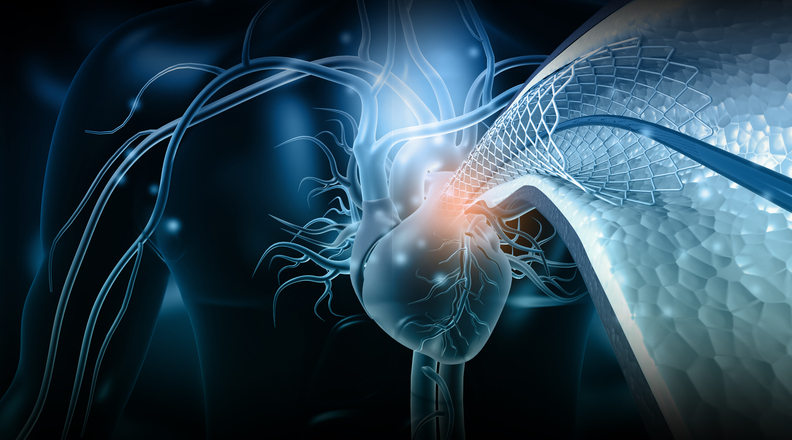
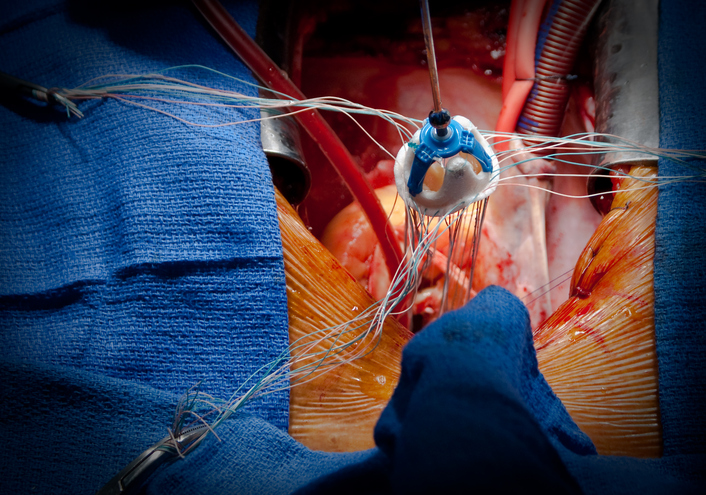
Recommendations for post-PCI antithrombotic therapy have been rapidly evolving, driven by equally fast-paced advancements in biomaterial science and coronary stent technology. The shift from bare metal stents to early-generation drug-eluting stents (DES) led to increased risk of in-stent thrombosis, driving rapid intensification of antiplatelet therapy recommendations with longer use of higher potency antiplatelets. With improved stent design, including the use of ultrathin struts and bioresorbable polymer, thrombotic complications lessened. The advent of newer-generation stents with fewer ischemic complications and increased recognition of the morbidity and mortality associated with bleeding complications drove studies investigating shorter DAPT duration, P2Y12 inhibitor de-escalation, and earlier transition to antiplatelet monotherapy, in both stable coronary disease and acute coronary syndromes, particularly in patients with high bleeding risk.
The T-PASS trial was an open-label, multicenter, randomized, controlled trial performed in Korea that sought to determine if short-term DAPT (<1 month) followed by ticagrelor monotherapy is noninferior and potentially superior to 12 months of ticagrelor-based DAPT in terms of ischemic and bleeding outcomes. Investigators enrolled 2850 patients presenting with ACS (mean age, 61 years; 17% women; 40% with STEMI; all from 1 of 24 Korean hospitals) who underwent PCI with the Biotronik Orsiro sirolimus-eluting stent to receive either ticagrelor monotherapy after less than 1 month of DAPT (n=1426) or 12 months of DAPT (aspirin and ticagrelor; n=1424). Those on concurrent oral anticoagulation or who were deemed to have a high bleeding risk were excluded. In the monotherapy group, aspirin was discontinued after a median of 16 days.
At 12 months of follow-up, there was a 46% reduction in the primary end point of net adverse cardiovascular events (NACE; composite of all-cause death, nonfatal myocardial infarction [MI], in-stent thrombosis, stroke, and Bleeding Academic Research Consortium [BARC] bleeding 3 or 5) in the abbreviated DAPT group (2.8% vs 5.2%; hazard ratio [HR], 0.54; 95% CI, 0.37-0.80; P for noninferiority<.001; P for superiority=.002), driven by a reduction in bleeding events. The rate of major adverse cardiac and cerebrovascular events (MACCE; composite of all-cause death, nonfatal MI, in-stent thrombosis, or stroke) was similar in the 2 groups (1.8% vs 2.2%; P=.51). Expectedly, the rate of BARC bleeding 3 or 5 was significantly lower in the abbreviated DAPT group (1.2% vs 3.4%; HR, 0.35; 95% CI, 0.20-0.61; P<.001).
In short, less than 1 month of DAPT (median, 16 days) followed by ticagrelor monotherapy in patients with ACS treated with the Orsiro DES led to fewer bleeding complications without excess ischemic events when compared with the standard 12 months of DAPT, despite excluding patients with high bleeding risk.
T-PASS builds on several recent trials studying abbreviated DAPT durations as improved stent designs drive an active retraction from earlier efforts to intensify antithrombotic therapies. Earlier trials adjudicated the safety and efficacy of 6-month DAPT duration following PCI for stable coronary disease. More recent trials began pushing the envelope further with even more abbreviated DAPT durations followed by antiplatelet monotherapy in a variety of populations spanning stable coronary disease to ACS, including ST-segment elevation myocardial infarction (STEMI).
Two trials looked at abbreviated DAPT followed by aspirin monotherapy:
- REDUCE-ACS (2019) showed that 3 months of DAPT followed by aspirin monotherapy was noninferior to 12 months of DAPT in the rate of NACE (composite of ischemic and bleeding outcomes) in 1460 patients with ACS (47% STEMI).
- ONE-MONTH DAPT (2021) showed that 1 month of DAPT followed by aspirin monotherapy was noninferior to 6 to 12 months of DAPT in the rate of NACE in 3020 patients with stable ischemic heart disease or unstable angina.
Three trials investigated 3 months of DAPT followed by P2Y12 monotherapy:
- SMART-CHOICE (2019) showed that 3 months of DAPT followed by P2Y12 monotherapy (mostly with clopidogrel) was noninferior in rates of MACCE at 1 year but led to significantly lower bleeding rates compared with 12 months of DAPT in 2993 patients (58% ACS; 11% STEMI).
- TWILIGHT (2019) showed that 3 months of DAPT followed by ticagrelor monotherapy led to significantly fewer bleeding events without a difference in ischemic events compared with 12 months of DAPT in 7119 patients (64% ACS; 0% STEMI).
- TICO (2020) showed that 3 months of DAPT followed by ticagrelor monotherapy led to significantly fewer bleeding events without a difference in ischemic events compared with 12 months of DAPT in an exclusively ACS population, including STEMI (n=3056; 100% ACS; 36% STEMI).
Three trials tested 1 month of DAPT followed by P2Y12 monotherapy:
- GLOBAL LEADERS (2018) showed no difference in rates of either all-cause death or MI, or bleeding rates with 1 month of DAPT followed by 23 months of ticagrelor versus 12 months of DAPT followed by aspirin monotherapy in 15,968 patients (47% ACS; 13% STEMI).
- STOPDAPT-2 (2019) showed that 1 month of DAPT followed by clopidogrel monotherapy was noninferior for both NACE and MACCE but resulted in lower bleeding compared with 12 months of DAPT in 3009 patients (38% ACS; 18% STEMI).
- STOPDAPT-2 ACS (2022) failed to show noninferiority of 1 to 2 months of DAPT followed by clopidogrel monotherapy versus 12 months of DAPT in rates of NACE in 4169 patients (76% ACS; 54% STEMI).
With advancements in stent technology and increasingly biocompatible platforms, the preponderance of evidence seems to advocate for short DAPT duration, even in the ACS population. Several questions remain. Generalizability with regards to ethnicity (T-PASS was conducted exclusively in Korea) and other stent platforms is uncertain. The merits of aspirin versus P2Y12 monotherapy are untested. The timing and optimal strategy of de-escalation after 1 year is also unknown. While we await future trials to clarify these questions, we can be certain that the tide is turning, and we should expect future guidelines to advocate for less intense antiplatelet strategies following PCI, regardless of bleeding risk.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.