
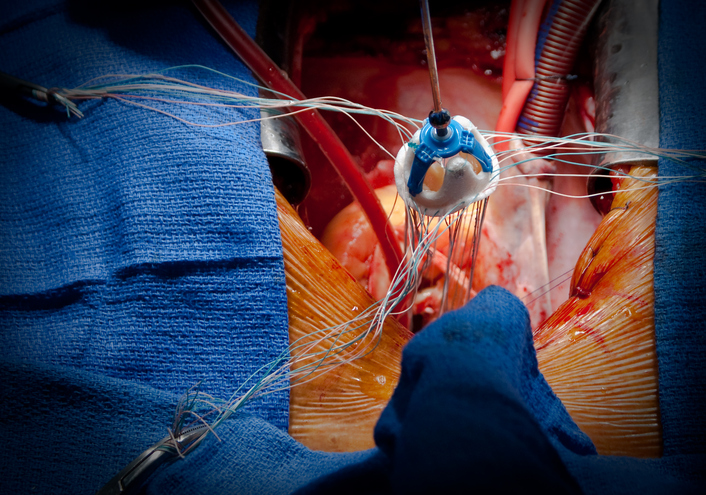
Orthotopic heart transplant(OHT) is the gold standard of treatment for end-stage heart failure patients.1 However, acute cardiac allograft rejection (ACAR) is the leading cause of mortality and morbidity in the first year after transplantation. These patients undergo routine surveillance endomyocardial biopsy (EMB) to assess for ACAR. Researchers from the St. Vincent Hospital, Sydney, report a novel methodology of using cardiac magnetic resonance (CMR) imaging to be similar to the EMB-based surveillance strategy.2
Researchers enrolled 33 OHT recipients in 2014; these patients underwent surveillance EMB, and CMR was done within 24 hours of EMB in the first year post-transplant to develop the validation cohort and compare it with healthy controls. Standard multiparametric T1 and T2-mapping cutoffs were defined for ACAR, which was used in the follow-up study. Thereafter, researchers performed a randomized, prospective, noninferiority study enrolling 20 patients in each arm comparing EMB or CMR-based surveillance 4 weeks after OHT. These patients underwent EMB or CMR-based surveillance at 4,6,8,10,12, 16,20,24, and 32 weeks after transplantation.2
In the validation cohort, the OHT recipients underwent 108 EMB and CMR and were compared with the healthy cohort. This study yielded receiver-operating-curve (ROC) analysis to identify high-grade rejection by CMR with an AUC of 0.897 for T1 and 0.938 for T2-mapping for high-grade rejection. There was high interobserver agreement and correlation for T1, T2, and interventricular septal and left ventricular global values. However, the sensitivity for detecting low-grade rejection by CMR was modest (AUC of 0.697 for T1 and 0.689 for T2).2
In the prospective cohort, CMR-based surveillance was non-inferior compared to EMB in 1-year follow-up in identifying high and low-grade rejection. Interestingly, there was no significant difference in the rate of infection events in both arms. The CMR group had less unplanned hospitalization (9 vs. 18, p<0.006) than the CMR group, but the median length of hospitalization was similar in both arms. Both groups also received similar immunosuppressive therapy. It is noteworthy that a remarkable decrease in the T1 and T2 levels were noted in the follow-up CMR of the patients who were found to have ACAR and received pulsed immunotherapy. And, there was a significant drop in the RV ejection fraction and an increased tricuspid regurgitation in the EMB arm.
Prominent CMR researcher and chief of Cardiology at the University of Virginia, Professor Dr. Christopher Kramer comments, “This is a very intriguing proof-of-principle single center study of the use of T1 and T2 mapping CMR to diagnose and treat myocardial transplant rejection. They demonstrated excellent accuracy of CMR parametric mapping for diagnosing ACAR in the derivation group. In the validation group, there were far fewer biopsies in the CMR group and no difference in events, although the numbers are small. This is essentially a feasibility study as concluded by the authors.
Strengths of the study include the careful study design and use of a derivation and validation cohorts and the randomization to no biopsy. Weaknesses include the single center nature and the small n, especially in the validation group, leading to possible beta error. Every scanner and field strength has different normal values for T1 and T2, making a multi-center study necessary, but difficult, to standardize these values across centers. Measurement of extracellular volume would normalize this across centers but requires gadolinium contrast infusion. Larger, multi-center studies are needed to make this concept a reality, but the promise is there and is quite exciting for transplant recipients, potentially avoiding the need for multiple biopsies.”
Great article by my colleague Dr Chris Anthony entitled Cardiovascular Magnetic Resonance for Rejection Surveillance After Cardiac Transplantation https://t.co/m1yyFRUwkJ @AllanLKleinMD1 @CleClinicMD @ASE360
— Allan L. Klein (@AllanLKleinMD1) June 1, 2022
https://twitter.com/faraonidmd/status/1531971374704631809?s=20&t=cRbWm14GQMes4iUFiRYJKw
References.
- Singh TP, Mehra MR, Gauvreau K. Long-Term Survival After Heart Transplantation at Centers Stratified by Short-Term Performance. Circulation: Heart Failure. 2019;12(11):e005914.
- Anthony C, Imran M, Pouliopoulos J, et al. Cardiovascular Magnetic Resonance for Rejection Surveillance After Cardiac Transplantation. Circulation.0(0):10.1161/CIRCULATIONAHA.1121.057006.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.